Desmoid tumors are complex and the information on this page is a general overview and not intended as medical advice for any individual problem, or as a diagnosis, treatment plan, or recommendation for a particular course of action, and this information should not be used as a substitute for professional medical advice and services. Please do not delay in seeking professional medical advice regarding your individual circumstances.
Signs & Symptoms
Symptoms can differ based on where the desmoid tumor is located in the body. Some patients will be able to actually feel a palpable lump or see swelling. By contrast, some patients may have no symptoms at all and no visible physical manifestation of the tumor. Below are some other common signs and symptoms associated with a desmoid tumor depending on location:
- Pain
- Swelling
- Visible deformities
- Cramping and nausea for abdominal tumors
- Impact on mobility
- Impact on bodily function such as urinary or bowel function, breathing, or swallowing
- Fatigue
Pathology
To make a definitive diagnosis, a biopsy is performed to collect a sample of tumor tissue that is then examined by a pathologist in a lab. Using a microscope, a pathologist can look for characteristics of desmoid tumor cells, which include moderately cellular, infiltrative spindle cell proliferations that are set in a collagenous stroma. Desmoid tumors are rare. Unfortunately, due to the complexities in sarcoma pathology, a misdiagnosis is possible in the pathology process. A second opinion by an expert soft tissue pathologist is recommended to confirm a desmoid tumor diagnosis.1
See what a desmoid tumor looks like when viewed under a microscope:
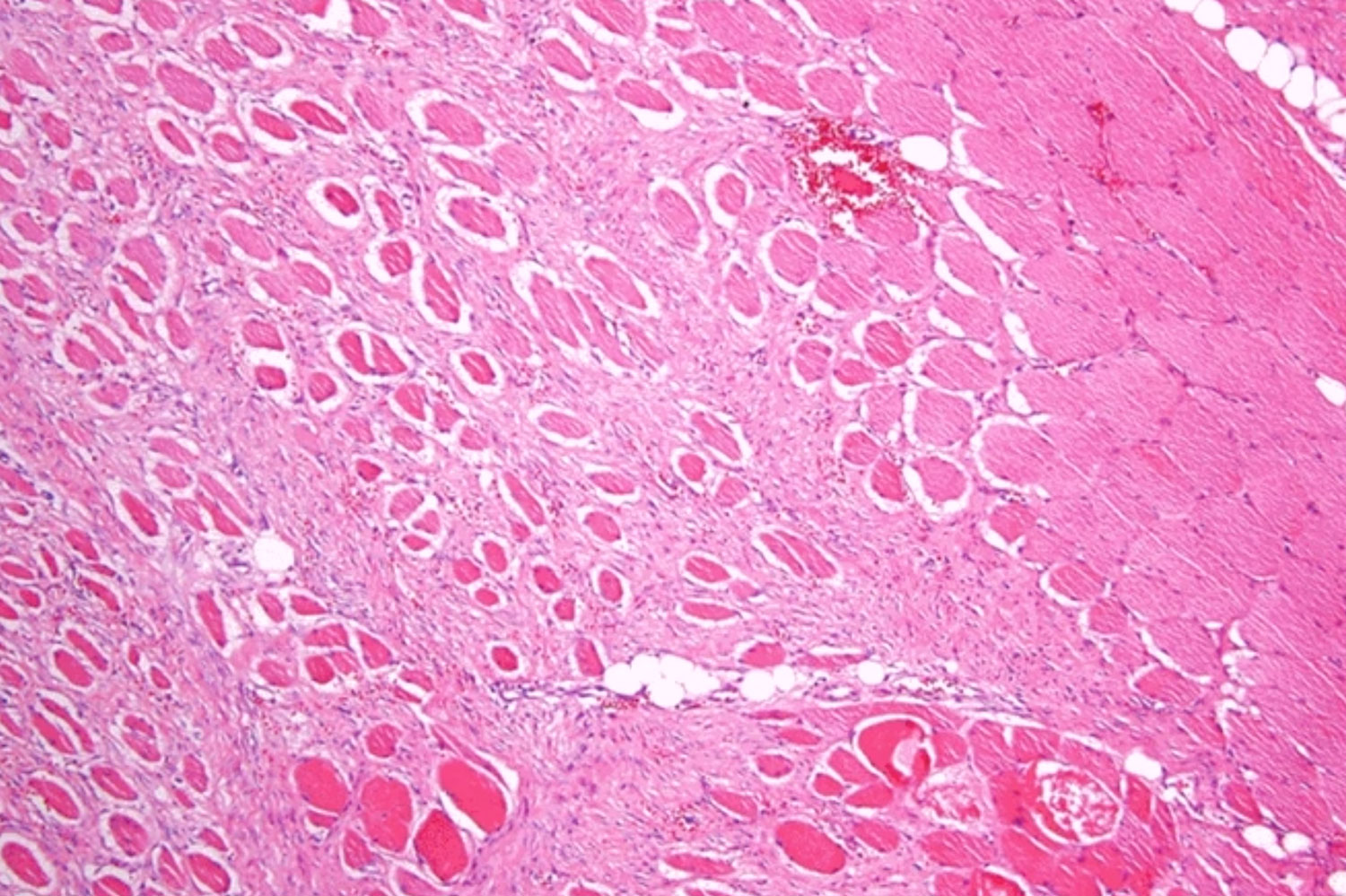
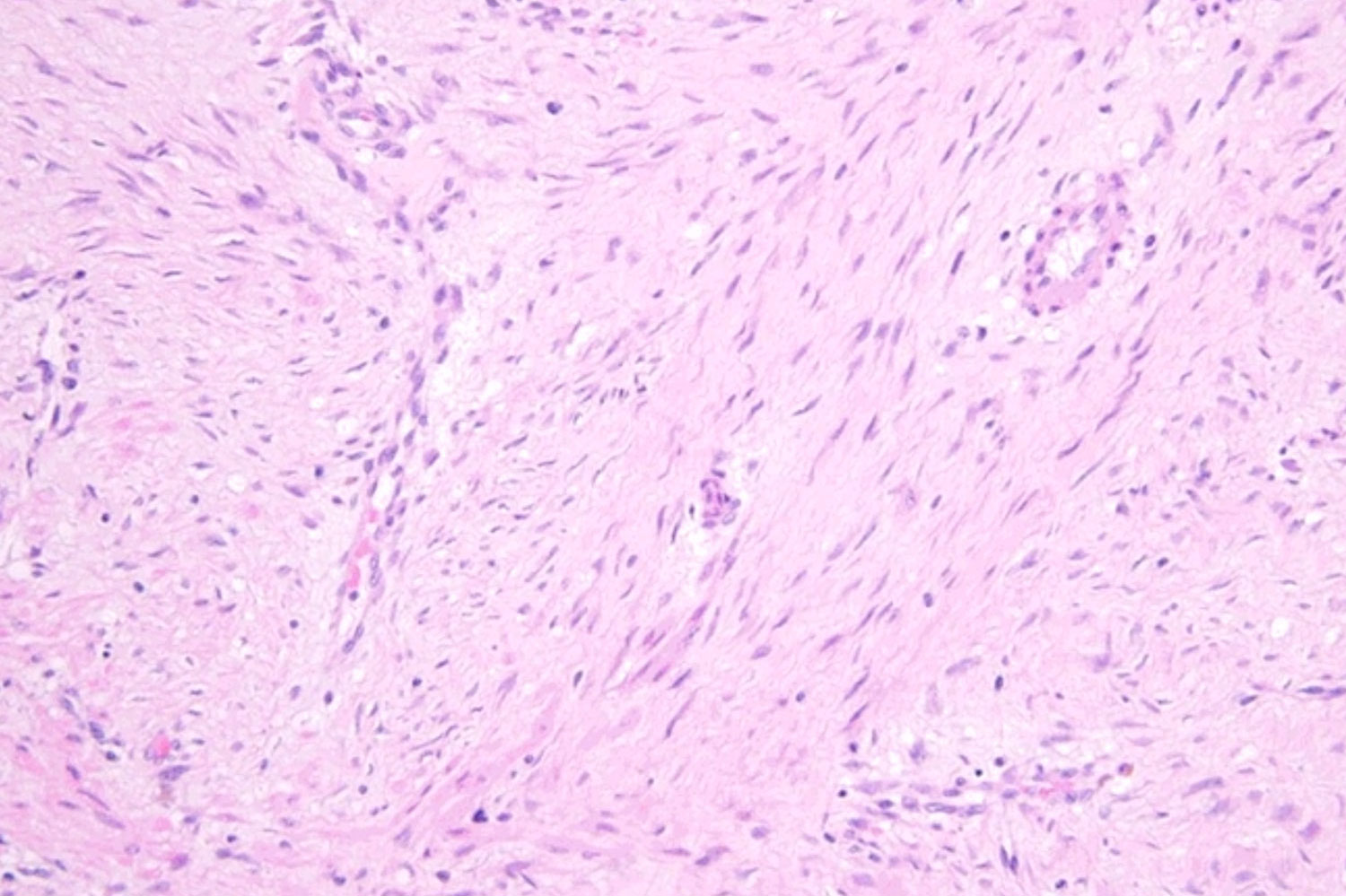
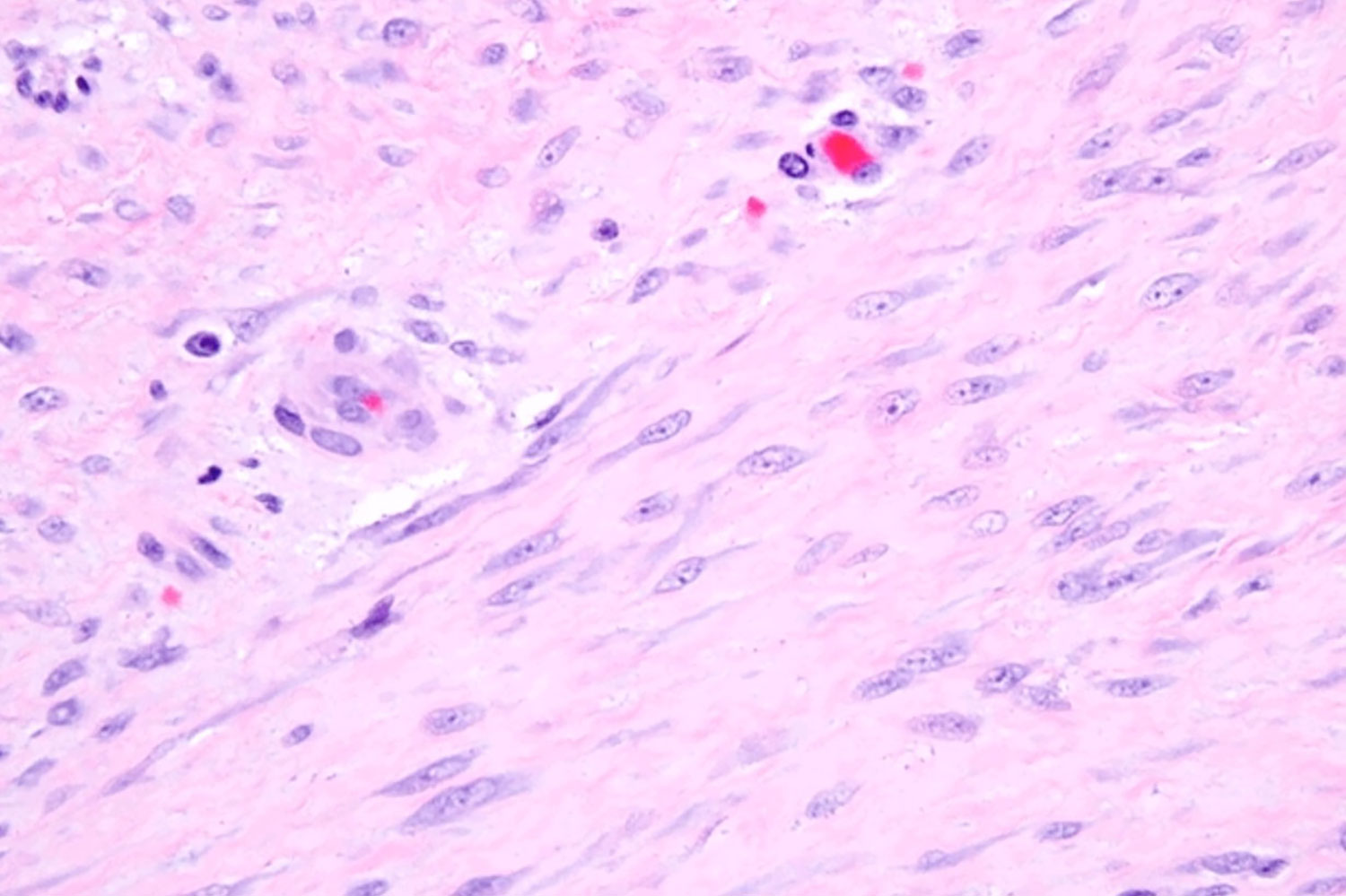
Images above were taken from SARC’s “Differential Diagnosis of Spindle Cell Sarcomas including Leiomyosarcoma”
Find a Sarcoma Expert
It is important to seek out a sarcoma specialist where possible, as they are more likely to be knowledgeable about desmoid tumor diagnosis and care. Sarcoma specialists can typically be found at major sarcoma centers within or affiliated with academic medical centers and can help support patient care through a multidisciplinary medical team, often forming what is called a tumor board.
“Mock Tumor Board”
with UPMC Experts - 2022 DTRF Patient Meeting Webinar #2
Imaging of Desmoid Tumors
Physicians can monitor, measure, and support the diagnosis of a desmoid tumor through a magnetic resonance imaging (MRI) scan. In most cases, MRI is generally the imaging modality of choice for desmoid tumors. MRIs have superior soft tissue contrast compared to computed tomography (CT) scans. In other words, most desmoid tumors are easier to see on an MRI against a background of other soft tissues such as muscle.
Learn more about imaging desmoid tumors on the Treatment & Monitoring page.
Need a Second Opinion?
Many doctors, even oncologists, may not be familiar with or have experience in treating desmoid tumors. Sometimes, it may make sense to get a second opinion to provide you with more information and choices regarding approach to treatment. Advocating for yourself or your loved one is a powerful tool and can help ensure you’re getting the right care.
The video below is a resource that can help answer your questions about your first clinical consultation and guide next steps.
LIVE: “Getting the Most Out of Your Consultation and Treatment Plan”
with Dr. Candace Haddox from Dana-Farber Cancer Institute (2022)
Misdiagnosis
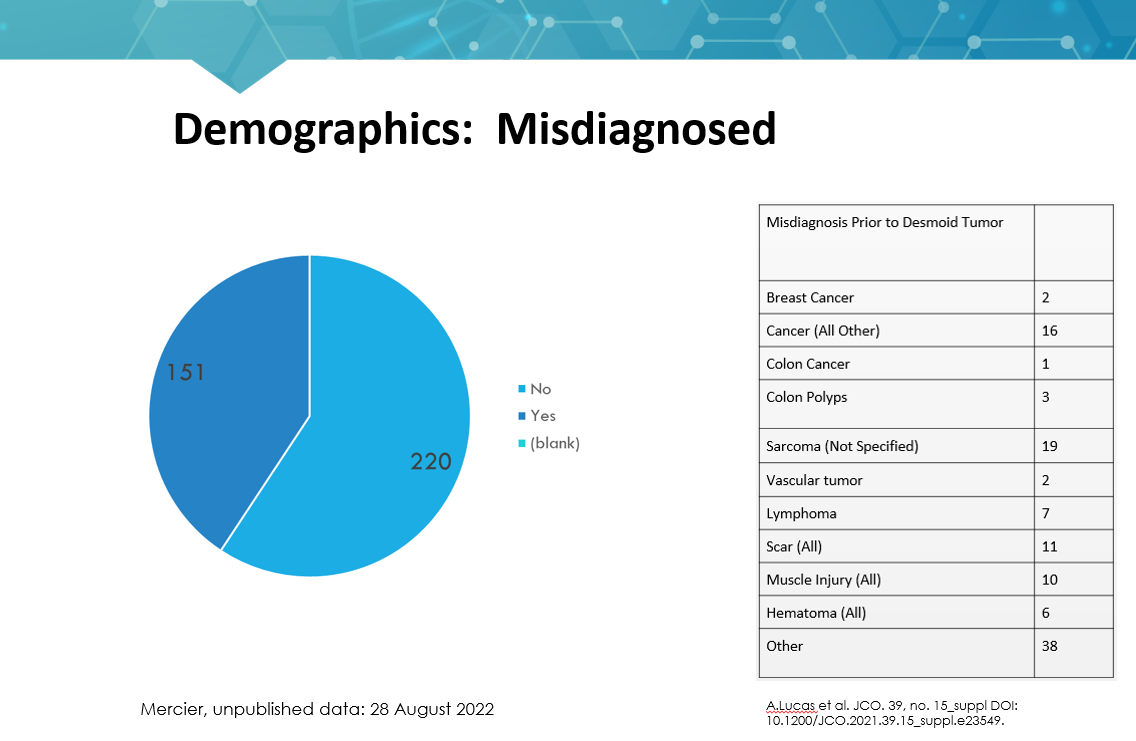
Because desmoid tumors are rare, cases can be misdiagnosed at the points of clinical examination, pathology, imaging or others. They are often misdiagnosed clinically as other more common or even benign diseases. See the graphic below for more information on the misdiagnosis of desmoid tumors. This graphic supports why an accurate pathology review by a soft tissue pathologist1 is critically important.
Treatment Options
The treatment of desmoid tumors can be complex, and what works for one person may not necessarily work for another.
Continue Exploring

Global Consensus Paper

Clinical Trials

Tissue Donation

References
- Constantinidou A, Scurr M, Judson I, Litchman C. Clinical presentation of desmoid tumors. In: Litchman C, ed. Desmoid Tumors. Springer; 2012:chap 2. Accessed March 29, 2023. https://www.researchgate.net/publication/226455135.
- Gounder MM, Maddux L, Paty J, Atkinson TM. Prospective development of a patient-reported outcomes instrument for desmoid tumors or aggressive fibromatosis. Cancer. 2020;126(3):531-539.
- Alman B, Attia S, Baumgarten C, et al. The management of desmoid tumours: A joint global consensus-based guideline approach for adult and paediatric patients. European Journal of Cancer. 2020. 127: 96-107. Access April 5, 2023. https://www.sciencedirect.com/science/article/pii/S0959804919308329.
- Penel, Nicolasa; Chibon, Frédéricb; Salas, Sébastienc. Adult desmoid tumors: biology, management and ongoing trials. Current Opinion in Oncology 29(4):p 268-274, July 2017. | DOI: 10.1097/CCO.0000000000000374
- Devezas V, Barbosa LE, Ramalho R, Sarmento C, Maia JC. Large desmoid tumors in familial adenomatous polyposis: a successful outcome. Autops Case Rep. 2018 Sep 26;8(4):e2018045. doi: 10.4322/acr.2018.045. PMID: 30775322; PMCID: PMC6360820.8